Diabetes affects about 1.5 million individuals in Australia. Diabetic retinopathy is one of the leading causes of visual loss in persons of working age. Because more individuals are being diagnosed with diabetes, the incidence of diabetic retinopathy has seen a large rise over the past 20 years. This growth can be attributed to the rise in the prevalence of diabetes.
We have taken due diligence to publish articles such as this to help you live a healthy life. Our Personal Eye doctors are professionals who create a medium for eye health through the best laser eye surgery, various laser treatments, and surgeries in New South Wales and the rest of Australia.
Eye patients have been choosing eye drops, intravitreal injections, and surgeries such as pterygium surgery, LASIK surgery, and other latest technology for their eye conditions. we hope that you will find this post about diabetic retinopathy, which was written by our refractive surgeons, resourceful.
What Kind of Damage Can Diabetes Cause to The Retina?
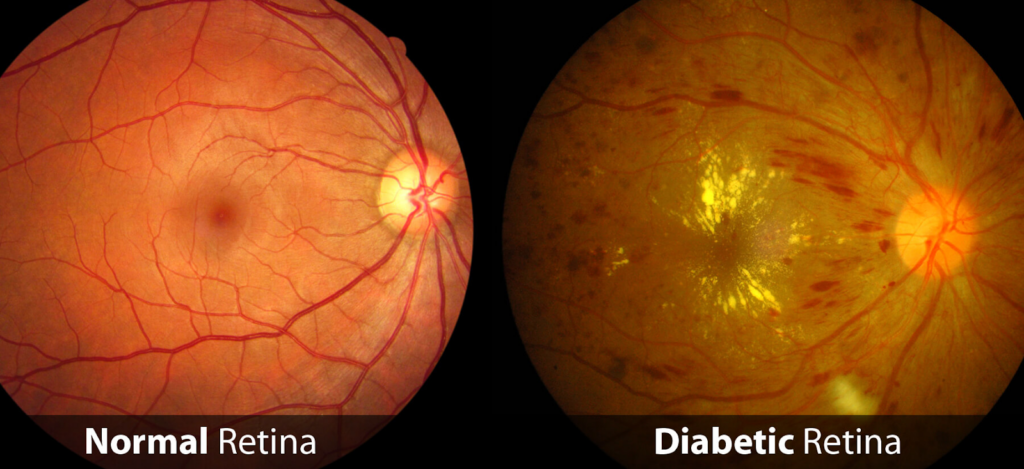
In the back of the eye lies a layer called the retina, which has the function of perceiving light. It is made up of blood vessels, nerve cells (neurones), and specialised cells called photoreceptors, which are involved in directly perceiving light.
The retina’s capacity to detect light requires energy, which in turn is dependent on the oxygen that is delivered by the blood as it circulates through the blood vessels.
The blood vessels of the retina get damaged when diabetes is present due to high blood sugar levels. Ischemia of the retina is the result of these damaged blood vessels, which also cause bleeding and do not provide the retina with the necessary amount of oxygen.
As a direct consequence of this, retinal cells start to die, and the retina loses its ability to perform its normal functions. In addition to this, diabetes causes direct damage to the neurons that make up the retina. These consequences, taken together, can lead to diabetic retinopathy.
It’s possible that diabetic retinopathy will first impact your central vision due to a disease known as diabetic macular edema. This is one of the causes of vision loss linked with diabetic retinopathy. This enlargement of the macula, which is a region of the retina responsible for clear vision in the center of the field of view, can lead to vision that is fuzzy and can distort pictures.
The growth of abnormal blood vessels, which can bleed within the eye and lead to a fast loss of vision, is a hallmark of advanced diabetic retinopathy. This condition is caused by diabetes. As the blood fills up the interior of the eye, this causes a rapid and dramatic loss of vision, similar to the appearance of a curtain.
If left untreated, diabetic retinopathy at its advanced stage can lead to retinal detachment, an emergency condition that calls for immediate surgical intervention and has the potential to cause irreparable and permanent vision loss if it is not addressed right away.
What measures can I take to protect my eyes against diabetic retinopathy?
It is recommended by the American Diabetes Association that most persons with diabetes keep their A1c level (a measurement of average blood sugar levels over the preceding two to three months) below 7% in order to reduce their chance of developing complications from diabetes.
As a result of the fact that glucose in the blood directly harms the blood vessels in the retina, there is compelling epidemiological evidence suggesting that maintaining healthy blood sugar levels leads to a reduction in both the incidence and severity of diabetic retinopathy.

It is recommended that people with diabetes achieve and keep their blood pressure in the normal range in order to lessen the risk of developing cardiovascular and microvascular complications of the disease. These complications include retinopathy, nephropathy (kidney disease), and neuropathy (nerve damage).
It is known that lowering blood pressure can postpone the formation of diabetic retinopathy, but it is unknown whether or not managing blood pressure can influence the progression of diabetic retinopathy once it has already developed.
In a similar vein, regulating cholesterol is recommended as part of overall diabetes treatment; however, it is unclear whether or whether doing so lowers the incidence of diabetic retinopathy.
What Are the Symptoms of Diabetic Retinopathy, and How Do You Tell Whether You Have Them?
Before there is any impairment to vision, an ophthalmologist can detect diabetic retinopathy and initiate treatment for it. In general, patients who have type 1 diabetes should visit an ophthalmologist once every year, commencing five years following the commencement of their condition. This recommendation applies to both children and adults.
People who have been diagnosed with type 2 diabetes should make an appointment with an ophthalmologist as soon as possible to have a retinal exam, and then they should continue to have yearly check-ups after that. If you are pregnant or have diabetic retinopathy that has progressed to a more severe stage, you may need to visit an ophthalmologist more regularly for cataract surgery or otherwise.
What can You do to Prevent or Slow Down the Progression of Your Visual Loss?

As was just discussed, when the blood vessels are damaged, the oxygen supply to the retina is cut off. The creation of a signal protein known as vascular endothelial growth factor (VEGF) is triggered when there is insufficient oxygen. The Harvard Medical School was the institution that made the initial discovery of VEGF and its function in eye illness.
There are drugs available today that have the ability to bind VEGF and, as a result, ameliorate the symptoms of diabetic retinopathy. These “anti-VEGF” drugs are injected directly into the eye and have the potential to ameliorate diabetic macular edema. In certain cases, they may potentially reduce the severity of diabetic retinopathy.
Steroids injected directly into the eye of certain patients may also be effective in improving diabetic macular edema. Patients with advanced cases of proliferative diabetic retinopathy, the most advanced form of diabetic retinopathy, may require retinal laser therapy or retinal surgery in order to stop or slow bleeding and leakage, shrink damaged blood vessels, or remove blood and scar tissue. Proliferative diabetic retinopathy is the most advanced form of diabetic retinopathy.
Lastly
If you are having any questions or inquiries about how to have correct vision, cataract surgery, Laser eye surgery, laser vision correction, diabetic retinopathy, minimally invasive glaucoma surgery, normally clear lens, vision loss, retinal conditions, short-sightedness, – you should get in touch with us via our Personal Eyes website to book your free assessment today.
Consider the factors outlined in this blog post, weigh the pros and cons, and most importantly, consult with a Sydney cataract surgeon at Personal Eyes before making the final decision.
